Abstract
The world's biggest threat to development and public health is HIV. Youth in sub-Saharan Africa are primarily affected by the HIV epidemic. Despite the availability of HIV prevention options, new infections among youth in Kenya only reduced by 56% between 2015 and 2021. Various HIV prevention interventions have been implemented among youth with little or no assessment of their effectiveness in reducing new HIV infections. The objective of the study was to evaluate the effect comprehensive HIV prevention information package of the package on syphilis infections levels among the youths in Kakamega and Kericho counties, Kenya. A non-randomized control trial was conducted with Kakamega as intervention and Kericho as Comparison County. The pretest questionnaire was administered in both intervention and control counties in December 2001. The posttest questionnaire was administered in both intervention and control counties after nine months of providing HIV prevention information package. Quantitative data was analyzed using descriptive and inferential statistics. Qualitative data was transcribed and analyzed thematically. There was significant increase in knowledge of sexually transmitted infections in intervention county (t = 3.340, P = 0.021). There was significant number of youth in Kakamega county who reported unusual sores in genital area at endline (t = 2.035, P = 0.043). Similarly, more youths sought treatment after experiencing the syphilis symptoms (t = 1.931, P = 0.054) at endline in Kakamega county. There were no significant differences in the number of youths in Kericho county at endline who experienced unusual symptoms, sought treatment and informed their sexual partners (P > 0.05). The findings from the study will inform national rollout of the intervention to contribute to safer sexual behaviors among youth.
Keywords
Comprehensive, Non-Randomized, Sexual Behavior, Syphilis Infection
1. Introduction
Human immuno-deficiency virus (HIV) is the World’s most significant challenge in public health. Efforts to reduce new HIV infections to fewer than 370 000 worldwide by 2025 have been off-track. Globally, over 1.5 million people became newly infected with HIV in 2021 compared with 1.6 million in 2019 representing 7% decline. Approximately 400 000 young people aged 15 -24 years in the world were newly infected with HIV in 2021 down from 450 000 in 2019
| [1] | UNAIDS. HIV Estimates. Joint United Nations Programme on HIV/AIDS, 2022. |
[1]
.
An estimated 269 000 young people aged 15-24 years got newly infected in 2021 in the Sub-Saharan region down from 332 100 in 2019. The East and South African region had the highest reduction in new HIV infections at 38% since 2010. An estimated 220 000 youth got newly infected in 2021 in the region down from 250 000 in 2019
| [1] | UNAIDS. HIV Estimates. Joint United Nations Programme on HIV/AIDS, 2022. |
[1]
. Only 30% males and 19% females aged 15-24 in sub–Saharan Africa have comprehensive knowledge on HIV. The Median condom use by men at last higher risk sex was only 58.6%, far from the global target of 90% by 2020
.
New HIV infections in Kenya have stabilized at an average of 34 540 people in 2021 down from 41 408 in 2019
| [3] | MOH. Kenya HIV Estimates Report. National AIDS Control Counci, 2022. |
[3]
. The youth contribute 42% of all new HIV infections in Kenya. The high new HIV infections can be attributed to casual sex with multiple partners, limited comprehensive information on HIV prevention and inconsistent and incorrect condom use. Only 42.6% of females and 69.6% of males aged 15-24 years with more than one sexual partner reported using a condom during their last sexual intercourse
| [4] | MOH. Kenya Demographic and Health survey Kenya National Bureau of Statistics, 2022. |
[4]
. Additionally, only 54% females and 55% males in this age group have comprehensive knowledge of HIV prevention
| [4] | MOH. Kenya Demographic and Health survey Kenya National Bureau of Statistics, 2022. |
[4]
. Achieving Kenya’s target of 75% reduction in adult new infections by 2025 demands effective and efficient delivery of HIV prevention interventions.
Kakamega and Kericho county have a projected population of 1 867 579 and 995 566
| [5] | KNBS. Kenya Population and Housing Census. Kenya National Bureau of Statistics, 2022. Available from www.knbs.or.ke |
[5]
. New HIV infections among youth in Kakamega and Kericho counties only reduced by 32 and 18.4% respectively between 2020 and 2022. Youths in Kakamega and Kericho counties contribute 31% and 39% of all new HIV infections in the county respectively
| [3] | MOH. Kenya HIV Estimates Report. National AIDS Control Counci, 2022. |
[3]
.
HIV prevention programs may not be taken up by young people if certain aspects of the health system, such as waiting times, provider attitudes, availability, and service costs, are present
| [6] | Crankshaw, T. L., Matthews, L., Giddy, J., Kaida, A., Ware, C. N., Smit, J., and Bangsberg, D. A conceptual framework for understanding HIV risk behavior in the context of supporting fertility goals among HIV-serodiscordant couples. Reproductive Health Matters, 20: sup39, 50-60, 2012. https://doi.org/10.1016/S0968-8080(12)39639 |
[6]
. A cross sectional study assessed predictors that influence the uptake of HIV services among youth aged 15~24 years in The Gambia. Using Anderson’s Model of Health Service Utilization, the predisposing factors (socio-demographic and HIV knowledge) and the need-for-care factors (sexual risk behaviors) predict healthcare utilization services
| [7] | Sonko, I., Chung, M. H., Hou, W. H., Chen, W. T., and Chang, P. C. Predictors of HIV service uptake among youth aged 15-24 years in The Gambia. PLoS One. 2022Feb 18; 17(2): e0263720. https://doi.org/10.1371/journal.pone.0263720 PMID: 35180256; PMCID: PMC8856544. |
[7]
.
Various HIV prevention interventions have been implemented among the youth with little or no assessment of their effect on risky sexual behavior. The study will inform the relevance and effectiveness of the strategies that the country is implementing in addressing risky sexual behavior among the youth. The comprehensive HIV prevention information package will empower the youth to make informed decisions concerning their risky sexual behavior and reduce their vulnerability to HIV infection. There is currently no effective HIV vaccine and reducing risky sexual behaviors among youth is essential in reducing their exposure to HIV infection. If we prevent new infections among youth, we will enhance health and productivity and reduce future treatment costs and ill-health liabilities at individual and family level. The study will provide new evidence to inform design and implementation of intervention to reduce risky sexual behavior among youth.
The objectives of the study were;
1. To determine the level of knowledge on sexually transmitted infections among youths in Kakamega and Kericho counties.
2. To evaluate the effect comprehensive HIV prevention information package of the package on syphilis infections levels among the youths in Kakamega and Kericho counties.
2. Materials and Methods
2.1. Study Design
A Nonrandomized control trial was conducted for 9 months from December 2021 using qualitative and quantitative methods. Nonrandomized control trials are typically much cheaper and may be more politically feasible to conduct
| [8] | Campbell, D. T., Stanley, J. Experimental and Quasi-Experimental Designs for Research. Houghton Mifflin, 1966. Boston, USA. |
[8]
.
2.2. Setting
The study was undertaken in Kakamega as intervention and Kericho as comparison county. These two were purposively selected because they are medium incidence
| [3] | MOH. Kenya HIV Estimates Report. National AIDS Control Counci, 2022. |
[3]
. The three sub counties in the two counties were randomly selected to represent urban, cosmopolitan and rural youth.
Nandi county is geographically located between Kakamega county (Intervention area) and Kericho county (Comparison area) to prevent effect of spillover or mixing of youth from the two study counties.
Kakamega and Kericho county have a projected population of 1 867 579 and 995 566
| [5] | KNBS. Kenya Population and Housing Census. Kenya National Bureau of Statistics, 2022. Available from www.knbs.or.ke |
[5]
. New HIV infections among young people in Kakamega and Kericho counties only reduced by 32 and 18.4% respectively between 2020 and 2022. Youth in Kakamega and Kericho counties contribute 31% and 39% of all new HIV infections in the county respectively
| [3] | MOH. Kenya HIV Estimates Report. National AIDS Control Counci, 2022. |
[3]
.
2.3. Study Population
The research population of interest were all youth in Kakamega and Kericho County. A target of 495 youth was the study subjects. The participants were selected from youth group meetings to represent out of school youth and from colleges and technical institutes to represent the in-school youth in the intervention and comparison county. Consenting youth residing in the intervention and control counties between December 2021 and September 2022 were the study participants.
2.4. Inclusion and Exclusion Criteria
1. Confirmed young person residing in the study counties for at least one year.
2. Youth aged 15 -24 years and able to give informed consent.
3. Youth below 18 years who assent in addition to parental consent.
2.5. Sampling
2.5.1. Sampling Strategy
The two counties, Kakamega and Kericho were purposively selected as intervention and comparison county. Stratified sampling was used to select three sub counties to represent urban, cosmopolitan and rural youth. Simple random sampling was used to select colleges or technical institutes to represent in-school youth and youth groups to represent out of school youth in the study counties. Individual youth who consented in both counties were invited to fill a questionnaire at baseline and after 9 months of providing comprehensive HIV prevention information package in the intervention county. Consecutive sampling was used to include all accessible individual study participants to provide information on the study questions. The change in uptake of condoms and HIV testing services in the intervention county was compared with the comparison county.
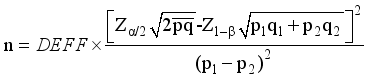
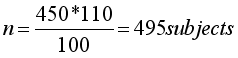
2.5.2. Sample Size Determination
For intervention studies,
| [9] | Suresh, K. P., Chandrashekara, S. Sample Size Estimation and Power Analysis for Clinical Research Studies. Journal of Human Reproductive Science, 2012; 5, 7-13. |
[9]
developed the following formula that was used to calculate a representative sample size for the study.
According to the Kenya Demographic and Health Survey, only 59% of youth in Kenya have comprehensive knowledge on HIV and AIDS
| [10] | MOH. Kenya Demographic and Health survey. Kenya National Bureau of Statistics, 2014. |
[10]
. We estimate that the intervention will increase comprehensive knowledge among this age group by 10%. Adjusting for 10% non-response rate
| [11] | Israel, G, D. Sampling The Evidence Of Extension Program Impact. IFAS, 1992. University of Florida. |
[11]
.
The sample size was 495 youth for the baseline survey and 495 in the follow-up survey. We will use stratified probability proportional to size (PPS) method
to obtain the number of young people to be sampled per county. The population of interest in each county was sampled proportional to its size.
Table 1. Sampling of youth from study count.
| County | Sub county | Youth | Sample |
1 | Kakamega | Lurambi | 42322 | 140 |
2 | Kakamega | Lugari | 25431 | 85 |
3 | Kakamega | Navakholo | 32100 | 106 |
| Sub total | | 99853 | 331 |
4 | Kericho | Ainamoi | 37122 | 68 |
5 | Kericho | Kipkelion East | 25638 | 47 |
6 | Kericho | Sigowet | 26724 | 49 |
| Sub total | 89484 | 164 |
| Total | | 495 |
2.5.3. Pre-Testing
Pre-test study was conducted using 50 youth in Machakos County that formed 10% of the sample size. Data was collected from 25 youth in a randomly selected sample of 3 youth groups and 25 young people from two Colleges or technical institutes in Machakos County. Data was collected through use of detailed questionnaire, structured interviews and some use of direct observation. The pretest county is medium incidence and was characteristically similar to participant counties. Pre-testing of instruments was also intended to improve clarity, precision, reliability and validity of data. Following analysis of the pretest study data, ambiguous or unclear questions were either be rephrased or removed.
2.5.4. Validity
A questionnaire was comprehensive enough to collect all the information needed to address the purpose and objectives of the study. A field test was conducted before the questionnaire was used for the pilot study. To test validity, the questionnaire was also be reviewed by my supervisors at Kenyatta University. Data from other sources was compared with results from this study. The findings from this study can be generalized for the effect comprehensive HIV prevention information package on risk sexual behavior among youth in Kenya.
2.5.5. Reliability
Pretesting the questionnaire helped enhance reliability of the instrument. The Research Assistants were trained on administering the research instruments. Reliability was established using a pilot test by collecting data from subjects not included in the sample. The same questionnaire was used during the interviews and all its subparts were measured using the same characteristic. To increase reliability of data collected, efforts for triangulation was undertaken including performing two separate interviews per county in addition to direct observation made.
2.6. Intervention
The comprehensive HIV prevention information package was provided to the youth in the intervention county after the baseline assessment. The HIV prevention information package had 3 contact sessions offered termly for 9 months. Each contact session was 3 hours long consisting of presentation, experience sharing, group discussion and practical demonstration. The package consisted of frequently asked questions on HIV and AIDS, overview of HIV including transmission and prevention options, condom use dialogue, key HIV and STIs messages and documentary. I trained two local peer facilitators on the comprehensive HIV Prevention information package to facilitate termly sessions with the youth. The out of school youth were meeting at the county Youth Empowerment center every last Saturday of the month to receive the intervention. Youthful HIV testing counselors from partner organizations were referred to the youth empowerment center to offer the service. Youth in the comparison county continued to receive routine HIV services offered at health facilities.
2.7. Data Collection
2.7.1. Data Collection Techniques
The quantitative data was collected from respondents at baseline and at endline after 9 months by using a self-administered questionnaires which had both structured and unstructured questions. Four key informant interviews were also conducted with program implementers to establish HIV prevention strategies available for young people. Six Focus Group Discussions with 8-10 youth was conducted for the qualitative study at baseline and at endline. A similar questionnaire was administered at baseline and end line period in both intervention and comparison county. The questionnaire also collected information on potential confounding factors such as age, gender, residence and other prevention programs that they had attended. The post test data was collected 9 months after implementing the comprehensive HIV prevention information package. Data was checked for completeness and internal consistency throughout the data collection period. The questionnaire together with participants’ responses was then coded and entered into a computer for analysis.
Figure 1. Intervention Flow Chart.
2.7.2. Data Collection Process
The quantitative data collection method involved individual interviews using pretested structured questionnaire that was well designed as per the research objectives. The trained research assistants asked all respondents to sign consent and assent form before participating in the study. Eligible participants who declined to participate were not coerced. The data collection process took 7 days at baseline and at endline in both intervention and comparison county. Each interview took an average of 45 minutes. The endline data was collected after 9 months of providing HIV Prevention information package to youth in the intervention county while youth in comparison county continued to receive routine health services. The researcher and research assistants analyzed the interview data and checked for inconsistencies and clarification.
The qualitative data was collected by conducting individual indepth interviews and focus group discussions. The reasearcher conducted 4 Key informant interview guides with key youth program implementers and 6 focus group discussions with youths per county. After explaining the study objectives and obtaining consent from respondents, the researcher requested permission to record and take notes during the session. Participants were assured of confidentiality and the information provided will be strictly used for the study. Participants were asked to respect each other’s opinion since there was no wrong response during the session. The researcher moderated the one hour discussion with participants while the research assistant took notes. The researcher finally thanked participants for their time.
2.8. Data Analysis
The qualitative data was transcribed and translated then entered into NVivo qualitative data software for coding and further analysis. The quantitative data was entered into SPSS and analyzed using descriptive statistics. These include mean, median, frequencies and standard deviation. The Difference-In-Difference (DID) regression model was used to compare outcomes between intervention and comparison county at baseline and after 9 months of the intervention at end line. A Chi square test was used to determine the effect of the comprehensive HIV prevention information package and testing for any significant difference. Potential confounders were measured at baseline and end line.
2.9. Ethical Considerations
Research proposal was approved by Kenyatta University Ethical Review Committee as No. PKU/2302/11441 before start of the study. The research permit was obtained from NACOSTI. Kakamega and Kericho counties gave clearance to collect data from colleges and youth groups. Written informed consent was obtained from all the study participants. Parental permission for adolescents aged 15-17 years was sought first before the minor’s assent was sought. No participant name appeared on the questionnaire. Participants were informed that there will be no penalties for declining to participate or for withdrawing from the study in the course of data collection and that no invasive procedures will be used. Access to database was restricted by password. Completed questionnaires were kept in lockable office.
3. Results
3.1. Demographic Information of the Sampled Population
A total of 495 respondents from Kericho and Kakamega were involved in this study with 100% response rate. Most of the respondents were from Kakamega (66.7%) based on the proportionate sample size. Both male and female young adults in the ages of 15 – 24 years were involved. Majority of the respondents 61.2% were in their tertiary education level and only 10.7% were married as summarized in
Table 2.
Table 2. Respondents’ demographic information.
Demographic information | Category | At Baseline (N = 495) | End line (N = 495) |
County | Kericho | 164 (33.1%) | 164 (33.1%) |
Kakamega | 331 (66.9%) | 331 (66.9%) |
Gender | Male | 233 (47.1%) | 233 (47.1%) |
Female | 262 (52.9%) | 262 (52.9%) |
Age (Years) | 15 – 19 | 185 (373.6%) | 183 (37.0%) |
20 – 24 | 306 (61.8%) | 312 (63.0%) |
Non -response | 3 (0.6%) | - |
Education level | None | 10 (2.0%) | 10 (2.0%) |
Primary | 58 (11.7%) | 26 (5.3%) |
Secondary | 113 (22.8%) | 95 (19.2%) |
Tertiary | 303 (61.2%) | 355 (71.7%) |
Non -response | 11 (2.2%) | 10 (2.0%) |
Religion | Christians | 456 (92.1%) | 466 (94.1%) |
Muslims | 32 (6.5%) | 26 (5.3%) |
Others | 3 (0.6%) | 2 (0.4%) |
Non -response | 4 (0.8%) | 1 (0.2%) |
Marital status | Married | 53 (10.7%) | 57 (11.5%) |
Single | 400 (80.8%) | 414 (83.6%) |
*Others | 34 (6.9%) | 21 (4.2%) |
Non -response | 8 (1.6%) | 3 (0.6%) |
3.2. Youths Knowledge on Sexually Transmitted Infections
Comparison of the youth’s knowledge on diseases transmission in the counties before and after interventions was conducted using a paired t-test. The findings showed that in Kakamega, there was a significant change in knowledge after intervention (t = 3.340, P = 0.021). In Kericho, there was no significant change (P > 0.05) as shown in
Table 3.
Table 3. Comparison of Knowledge on sexually transmitted infections in the two Counties.
Disease | Proportional response (%) |
Kakamega baseline (n =331) | Kakamega endline (n=331) | Kericho baseline (n =164) | Kericho endline (n =164) |
HIV | 223 (67.4) | 317 (95.8) | 121 (73.8) | 121 (73.8) |
Syphilis | 194 (58.6) | 312 (94.3) | 127 (77.4) | 122 (74.4) |
Gonorrhea | 163 (49.2) | 301 (90.9) | 94 (57.3) | 81 (49.4) |
Chlamydia | 44 (13.3) | 94 (28.45) | 22 (13.4) | 16 (9.8) |
Herpes simplex | 44 (13.3) | 78 (23.6) | 21 (12.8) | 10 (6.1) |
Others | 3 (0.91) | 3 (0.91) | 0 (0.0) | 7 (4.3) |
t value | 3.340 | 1.557 |
df | 5 | 5 |
P-value | 0.021* | 0.180 |
3.3. Level of Syphilis Infection in Kakamega and Kericho Counties
Comparison of levels of syphilis infection in the two counties revealed that, in Kakamega there was a significantly higher number of youths who were able to identify unusual sores in their genitalia area compared to the number at baseline (t = 2.035, P = 0.043). Similarly, significantly more youths sought treatment after experiencing the symptoms (t = 1.931, P = 0.054). In Kericho, there were no significant differences in the number of youths at endline to baseline who experienced unusual symptoms, sought treatment and informed their sexual partners (P > 0.05) as summarized in
Table 4.Table 4. Syphilis infections in Kakamega and Kericho counties at baseline and endline.
Statement | Kakamega baseline | Kakamega endline | t-value | P | Kericho baseline | Kericho endline | t-value | P |
Experienced unusual sore in genital area | 63 (70.0%) | 85 (70.2%) | 2.035 | 0.043 | 27 (30.0%) | 36 (29.8%) | 1.288 | 0.199 |
Sought treatment after symptoms | 73 (64.0%) | 98 (67.1%) | 1.931 | 0.054 | 41 (34.0%) | 48 (32.9%) | 0.854 | 0.394 |
Informed their sexual partners after experiencing symptoms | 104 (72.7%) | 114 (69.1%) | 0.384 | 0.701 | 39 (27.3%) | 51 (30.9%) | 1.506 | 0.134 |
3.4. Reasons for Youths Failure to Seek Treatment
The main reasons why the youth did not seek treatment of syphilis symptoms in Kakamega county were no money (27.3%), did not know they were sick (26.1%), did not have time to go to hospital (9.1%) and hospital do not treat such diseases (2.8%). For Kericho county, the main reasons for not seeking treatment of the syphilis symptoms were did not know they were sick (29.3%), no money (21.6%), did not have time to go to hospital (17.2%) and hospital do not treat such diseases (7.8%) as summarized in
table 5.
Table 5. Reasons for not seeking treatment.
| Proportional responses (%) |
Reasons | Kakamega | Kericho |
No money | 48 (27.3) | 25 (21.6) |
Do not have time to go to the hospital | 16 (9.1) | 20 (17.2) |
Hospital do not treat such diseases | 5 (2.8) | 9 (7.8) |
Do not know that was sick | 46 (26.1) | 34 (29.3) |
Other reasons | 61 (34.7) | 28 (24.1) |
t value | 0.848 |
P value | 0.069 |
4. Discussion
In Kakamega, the percentage of youths who experienced syphilis symptoms increased marginally to 70.2% at endline from 70.0% at baseline. For Kericho county, the percentage of youth who experienced syphilis symptoms reduced to 29.8% at the end of the survey from 30.0% at baseline. There was however significant difference in percentage youth in the intervention county who informed their sexual partners after experiencing syphilis symptoms (χ
2 = 9.695, p = 0.008). A similar HIV prevention program conducted among Thai men who had STIs did not improve participants’ usage of condoms with steady partners and never decreased the number of sexual partners and STI reinfection rate after 3-month follow-up
| [13] | Thato, R., Daengsaard, E., and Sukrak, N. The Effect of a Brief HIV Prevention Program on Risk Reduction Behaviors Among Thai Men Diagnosed With Sexually Transmitted Infections, Asian Nursing Research, Volume12, Issue 4, 2018, Pages 265- 272, ISSN 1976-1317, https://doi.org/10.1016/j.anr.2018.10.003 |
[13]
. The findings also concur with a study in South Africa that integrated economic strengthening and prevention HIV education interventions which did not significantly affect prevalence of sexually transmitted disease infection and behaviour among adolescents at endline
| [14] | Burke, H. M., Chen, M., and Murray, K. The effects of the integration of an economic strengthening and HIV prevention education programme on the prevalence of sexually transmitted infections and savings behaviours among adolescents: a full-factorial randomised controlled trial in South Africa BMJGlobaHealth 2020; 5: e002029. http://dx.doi.org/10.1136/bmjgh-2019-002029 |
[14]
. Majority of the respondents in a similar study did not inform their sexual partners when they experienced STIs symptoms, showing no significant variation by gender
| [15] | Khasewa J, Mwanzo I and Orago A: Risky sexual behaviour and associated factors among youth in Kakamega and Kericho counties, Kenya, African Journal of Health Sciences, Vol. 36 No. 1. http://dx.doi.org/10.4314/ajhs.v36i1.8 , 2023. |
[15]
. An education intervention implemented among Egyptian women at a primary care facility significantly increased STIs knowledge, prevention, treatment and attitude at endline
| [16] | Amin, T. T., Galal, Y. S., Shaheen, D. S., and Salem, M. R. The Effect of Educational Intervention on Knowledge and Attitudes toward Sexually Transmitted Infections on a Sample of Egyptian Women at Primary Care Level. Open Access Maced J Med Sci 2021 Feb. 12 [cited 2023 Oct. 10]; 9(E): 138-44. Available from: https://oamjms.eu/index.php/mjms/article/view/5638 |
[16]
.
5. Recommendations
1. Expand the minimum package for young people in the Fast Track plan to include key messages and Frequently asked questions on sexually transmitted infections
2. Utilize existing infrastructure and delivery platforms for national roll-out of the comprehensive HIV prevention package
6. Conclusions
The comprehensive HIV prevention information package was successful in increasing knowledge on sexually transmitted infections and youths reporting syphilis infection.
Abbreviations
AIDS | Acquired Immune Deficiency Virus |
AYP | Adolescent and Young People |
DID | Difference-in-Difference |
FGD | Focus Group Discussions |
HIV | Human Immunodeficiency Virus |
HTS | HIV Testing Services |
KDHS | Kenya Demographic and Health Survey |
KII | Key Informant Interview |
NACOSTI | National Commission for Science, Echnology and Innovations |
UNAIDS | Joint United Nations Programme on AIDS |
SPSS | Statistical Package for Social Sciences |
STI | Sexually Transmitted Infection |
TVET | Technical and Vocational Education and Training |
Acknowledgments
Authors wish to acknowledge Dr Chrispinus Wamalwa and Peter Cheruiyot for permission to conduct the research in TVET Colleges in Kakamega and Kericho counties. We appreciate the support of TVET Principals and the youths who agreed to participate in the study. Thanks to Lawrence Alaro, Joseph Wanyonyi, Aggrey Indeje, Sylvia Dianga,, Catherine Washira, Abdi Swaleh Geoffrey Kigen, Sylvia Chepngetich, George Dianga and Cyphrene Wasike for their assistance throughout this study. The support of the research Assistants Fatuma Maalim, Gideon Korir, Josephat Marumbu and Damaris Momanyi cannot be overemphasized.
Finally, my special thanks go to Leon and Fleming for staying with me until very late at night as I worked on this research.
Author Contributions
Joab Khasewa: Conceptualization, Methodology, Formal Analysis, Funding acquisition, Investigation, Visualization, Writing – original draft
Isaac Mwanzo: Supervision, Methodology, Data Curation, Funding acquisition, Validation, Visualization, Writing – review & editing
Alloys Orago: Supervision, Methodology, Data curation, Validation, Visualization, Writing – review & editing
Funding
This research was funded by Royal Society of Tropical Medicine and Hygiene (RSTMH) small grants programme.
Data Availability Statement
Data available upon writing to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
| [1] |
UNAIDS. HIV Estimates. Joint United Nations Programme on HIV/AIDS, 2022.
|
| [2] |
ICF. The DHS Program, ICF Internationa, 2018. Retrieved From
https://www.dhsprogram.com/
|
| [3] |
MOH. Kenya HIV Estimates Report. National AIDS Control Counci, 2022.
|
| [4] |
MOH. Kenya Demographic and Health survey Kenya National Bureau of Statistics, 2022.
|
| [5] |
KNBS. Kenya Population and Housing Census. Kenya National Bureau of Statistics, 2022. Available from
www.knbs.or.ke
|
| [6] |
Crankshaw, T. L., Matthews, L., Giddy, J., Kaida, A., Ware, C. N., Smit, J., and Bangsberg, D. A conceptual framework for understanding HIV risk behavior in the context of supporting fertility goals among HIV-serodiscordant couples. Reproductive Health Matters, 20: sup39, 50-60, 2012.
https://doi.org/10.1016/S0968-8080(12)39639
|
| [7] |
Sonko, I., Chung, M. H., Hou, W. H., Chen, W. T., and Chang, P. C. Predictors of HIV service uptake among youth aged 15-24 years in The Gambia. PLoS One. 2022Feb 18; 17(2): e0263720.
https://doi.org/10.1371/journal.pone.0263720
PMID: 35180256; PMCID: PMC8856544.
|
| [8] |
Campbell, D. T., Stanley, J. Experimental and Quasi-Experimental Designs for Research. Houghton Mifflin, 1966. Boston, USA.
|
| [9] |
Suresh, K. P., Chandrashekara, S. Sample Size Estimation and Power Analysis for Clinical Research Studies. Journal of Human Reproductive Science, 2012; 5, 7-13.
|
| [10] |
MOH. Kenya Demographic and Health survey. Kenya National Bureau of Statistics, 2014.
|
| [11] |
Israel, G, D. Sampling The Evidence Of Extension Program Impact. IFAS, 1992. University of Florida.
|
| [12] |
Cochran, W. G. Sampling Techniques, 2nd Ed. John Wiley and Sons Inc, 1963. New York, USA;
https://doi.org/10.1002/bimj.19650070312
|
| [13] |
Thato, R., Daengsaard, E., and Sukrak, N. The Effect of a Brief HIV Prevention Program on Risk Reduction Behaviors Among Thai Men Diagnosed With Sexually Transmitted Infections, Asian Nursing Research, Volume12, Issue 4, 2018, Pages 265- 272, ISSN 1976-1317,
https://doi.org/10.1016/j.anr.2018.10.003
|
| [14] |
Burke, H. M., Chen, M., and Murray, K. The effects of the integration of an economic strengthening and HIV prevention education programme on the prevalence of sexually transmitted infections and savings behaviours among adolescents: a full-factorial randomised controlled trial in South Africa BMJGlobaHealth 2020; 5: e002029.
http://dx.doi.org/10.1136/bmjgh-2019-002029
|
| [15] |
Khasewa J, Mwanzo I and Orago A: Risky sexual behaviour and associated factors among youth in Kakamega and Kericho counties, Kenya, African Journal of Health Sciences, Vol. 36 No. 1.
http://dx.doi.org/10.4314/ajhs.v36i1.8
, 2023.
|
| [16] |
Amin, T. T., Galal, Y. S., Shaheen, D. S., and Salem, M. R. The Effect of Educational Intervention on Knowledge and Attitudes toward Sexually Transmitted Infections on a Sample of Egyptian Women at Primary Care Level. Open Access Maced J Med Sci 2021 Feb. 12 [cited 2023 Oct. 10]; 9(E): 138-44. Available from:
https://oamjms.eu/index.php/mjms/article/view/5638
|
Cite This Article
-
APA Style
Khasewa, J., Mwanzo, I., Orago, A. (2024). Effect of Comprehensive HIV Prevention Information Package on Syphilis Infection Levels Among Youths in Kakamega and Kericho Counties, Kenya. Central African Journal of Public Health, 10(4), 188-195. https://doi.org/10.11648/j.cajph.20241004.14
 Copy
|
Copy
|
 Download
Download
ACS Style
Khasewa, J.; Mwanzo, I.; Orago, A. Effect of Comprehensive HIV Prevention Information Package on Syphilis Infection Levels Among Youths in Kakamega and Kericho Counties, Kenya. Cent. Afr. J. Public Health 2024, 10(4), 188-195. doi: 10.11648/j.cajph.20241004.14
 Copy
|
Copy
|
 Download
Download
AMA Style
Khasewa J, Mwanzo I, Orago A. Effect of Comprehensive HIV Prevention Information Package on Syphilis Infection Levels Among Youths in Kakamega and Kericho Counties, Kenya. Cent Afr J Public Health. 2024;10(4):188-195. doi: 10.11648/j.cajph.20241004.14
 Copy
|
Copy
|
 Download
Download
-
@article{10.11648/j.cajph.20241004.14,
author = {Joab Khasewa and Isaac Mwanzo and Alloys Orago},
title = {Effect of Comprehensive HIV Prevention Information Package on Syphilis Infection Levels Among Youths in Kakamega and Kericho Counties, Kenya
},
journal = {Central African Journal of Public Health},
volume = {10},
number = {4},
pages = {188-195},
doi = {10.11648/j.cajph.20241004.14},
url = {https://doi.org/10.11648/j.cajph.20241004.14},
eprint = {https://article.sciencepublishinggroup.com/pdf/10.11648.j.cajph.20241004.14},
abstract = {The world's biggest threat to development and public health is HIV. Youth in sub-Saharan Africa are primarily affected by the HIV epidemic. Despite the availability of HIV prevention options, new infections among youth in Kenya only reduced by 56% between 2015 and 2021. Various HIV prevention interventions have been implemented among youth with little or no assessment of their effectiveness in reducing new HIV infections. The objective of the study was to evaluate the effect comprehensive HIV prevention information package of the package on syphilis infections levels among the youths in Kakamega and Kericho counties, Kenya. A non-randomized control trial was conducted with Kakamega as intervention and Kericho as Comparison County. The pretest questionnaire was administered in both intervention and control counties in December 2001. The posttest questionnaire was administered in both intervention and control counties after nine months of providing HIV prevention information package. Quantitative data was analyzed using descriptive and inferential statistics. Qualitative data was transcribed and analyzed thematically. There was significant increase in knowledge of sexually transmitted infections in intervention county (t = 3.340, P = 0.021). There was significant number of youth in Kakamega county who reported unusual sores in genital area at endline (t = 2.035, P = 0.043). Similarly, more youths sought treatment after experiencing the syphilis symptoms (t = 1.931, P = 0.054) at endline in Kakamega county. There were no significant differences in the number of youths in Kericho county at endline who experienced unusual symptoms, sought treatment and informed their sexual partners (P > 0.05). The findings from the study will inform national rollout of the intervention to contribute to safer sexual behaviors among youth.
},
year = {2024}
}
 Copy
|
Copy
|
 Download
Download
-
TY - JOUR
T1 - Effect of Comprehensive HIV Prevention Information Package on Syphilis Infection Levels Among Youths in Kakamega and Kericho Counties, Kenya
AU - Joab Khasewa
AU - Isaac Mwanzo
AU - Alloys Orago
Y1 - 2024/08/30
PY - 2024
N1 - https://doi.org/10.11648/j.cajph.20241004.14
DO - 10.11648/j.cajph.20241004.14
T2 - Central African Journal of Public Health
JF - Central African Journal of Public Health
JO - Central African Journal of Public Health
SP - 188
EP - 195
PB - Science Publishing Group
SN - 2575-5781
UR - https://doi.org/10.11648/j.cajph.20241004.14
AB - The world's biggest threat to development and public health is HIV. Youth in sub-Saharan Africa are primarily affected by the HIV epidemic. Despite the availability of HIV prevention options, new infections among youth in Kenya only reduced by 56% between 2015 and 2021. Various HIV prevention interventions have been implemented among youth with little or no assessment of their effectiveness in reducing new HIV infections. The objective of the study was to evaluate the effect comprehensive HIV prevention information package of the package on syphilis infections levels among the youths in Kakamega and Kericho counties, Kenya. A non-randomized control trial was conducted with Kakamega as intervention and Kericho as Comparison County. The pretest questionnaire was administered in both intervention and control counties in December 2001. The posttest questionnaire was administered in both intervention and control counties after nine months of providing HIV prevention information package. Quantitative data was analyzed using descriptive and inferential statistics. Qualitative data was transcribed and analyzed thematically. There was significant increase in knowledge of sexually transmitted infections in intervention county (t = 3.340, P = 0.021). There was significant number of youth in Kakamega county who reported unusual sores in genital area at endline (t = 2.035, P = 0.043). Similarly, more youths sought treatment after experiencing the syphilis symptoms (t = 1.931, P = 0.054) at endline in Kakamega county. There were no significant differences in the number of youths in Kericho county at endline who experienced unusual symptoms, sought treatment and informed their sexual partners (P > 0.05). The findings from the study will inform national rollout of the intervention to contribute to safer sexual behaviors among youth.
VL - 10
IS - 4
ER -
 Copy
|
Copy
|
 Download
Download